For many newborns, particularly those born prematurely, maintaining stable respiratory function is a significant challenge. Traditional methods have often leaned heavily on mechanical ventilation, which, while effective, comes with its share of complications. An alternative that has garnered widespread acceptance due to its efficacy and gentleness is the Bubble Continuous Positive Airway Pressure Bubble CPAP system. This innovative approach offers substantial benefits in supporting the respiratory needs of newborns, particularly in enhancing lung function and promoting healthier breathing patterns.
Understanding Bubble CPAP
Bubble CPAP is a non-invasive ventilation strategy used primarily in neonatal intensive care units to assist infants who struggle with breathing on their own. This system delivers continuous positive airway pressure to the lungs, which helps keep them open and aids in the exchange of oxygen and carbon dioxide. Unlike mechanical ventilators, Bubble CPAP does not breathe for the infant but rather supports their spontaneous breathing, thus improving respiratory function and overall lung development.
How Bubble CPAP Works
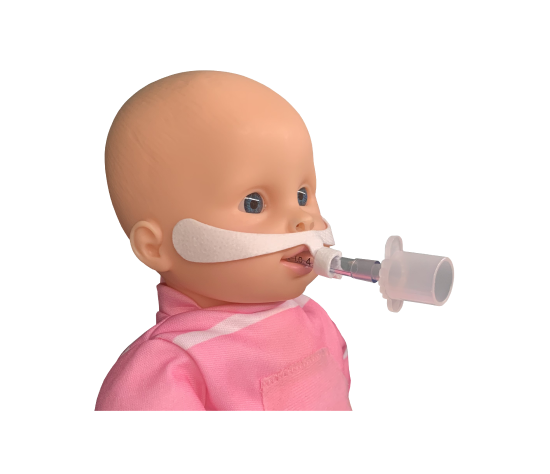
The mechanism behind Bubble CPAP involves delivering air, or a mix of air and oxygen, through nasal prongs or a mask. This airflow creates a ‘bubble’ effect as it exits through a tube partially submerged in water. The depth of the tube in the water determines the pressure level. This pressure maintains small airways open, prevents alveolar collapse at the end of expiration, and reduces the work of breathing. By stabilizing the air sacs in the lungs, Bubble CPAP ensures more consistent oxygenation and better carbon dioxide elimination.
Key Benefits of Bubble CPAP for Respiratory Function
Enhanced Lung Compliance: One of the primary benefits of Bubble CPAP is the improvement in lung compliance. It helps the lungs become more flexible and responsive to small volumes of air, which is essential for effective breathing. This increased compliance reduces the energy newborns expend on breathing, preserving their energy for growth and recovery.
- Prevention of Atelectasis: Atelectasis, or the collapse of lung tissue, is a common issue in newborns with respiratory distress. Bubble CPAP prevents the collapse of the alveoli (air sacs within the lungs) and helps maintain functional residual capacity, thus promoting better gas exchange and reducing the risk of lung tissue damage.
- Improved Oxygenation: By keeping the airways open and supporting the alveoli, Bubble CPAP improves the oxygenation of the blood. This is crucial for the survival and healthy development of the infant, particularly for those with compromised lung function.
- Decreased Need for Mechanical Ventilation: Using Bubble CPAP can often decrease the necessity for more invasive forms of respiratory support like mechanical ventilation, which can lead to complications such as ventilator-associated pneumonia or lung injury.
- Synchronization with Infant’s Breathing Efforts: Bubble CPAP synchronizes with the infant’s own respiratory efforts, promoting a more physiological breathing pattern. This synchronization helps to strengthen the respiratory muscles and improves the newborn’s ability to breathe independently over time.
Clinical Outcomes and Research Support
Research and clinical trials have consistently supported the use of Bubble CPAP for improving respiratory outcomes in newborns. Studies have shown that infants treated with Bubble CPAP have lower rates of respiratory failure and less need for subsequent mechanical ventilation compared to those who receive only conventional oxygen therapy. Additionally, the use of Bubble CPAP has been associated with a reduction in the incidence of bronchopulmonary dysplasia, a chronic lung condition that can develop in premature infants.
Implementing Bubble CPAP
The implementation of Bubble CPAP should be carried out by trained neonatal care providers. The settings – such as the pressure of the airflow and the composition of the gas mixture – need to be carefully adjusted based on the infant’s respiratory status and overall condition. Monitoring and adjustments are critical to ensure the effectiveness of the treatment and the safety of the infant.
Bubble CPAP is a specialized form of respiratory support widely used in neonatal care to enhance the breathing of newborns experiencing respiratory distress. This method utilizes a system where CPAP newborns breathe through nasal prongs connected to a tube submerged in water, creating pressure through bubbles. The consistent, gentle pressure maintained by the bubble CPAP system helps keep the newborns’ airways open, thus improving gas exchange and oxygenation. For CPAP newborns, this method is less invasive and can reduce the need for mechanical ventilation, which can be more traumatic. Bubble CPAP has proven particularly beneficial, helping newborns CPAP strengthen their lung function and reduce the incidence of lung injury.
Conclusion
Bubble CPAP represents a significant advancement in the care of newborns with respiratory distress. By enhancing respiratory function through non-invasive methods, it provides a safer and often more effective alternative to mechanical ventilation for CPAP newborns. For healthcare providers, parents, and caregivers of CPAP newborns, comprehending how Bubble CPAP benefits respiratory function is essential. This understanding can lead to more informed treatment decisions and improved outcomes for CPAP newborns. Embracing this technology ensures that the most vulnerable patients receive the best possible care, optimizing their recovery and growth during critical early life stages.