Parents often hear “saline” mentioned alongside inhaled treatments, then get stuck on one practical question. How many milliliters should be placed in the cup so therapy runs correctly, and the baby tolerates it? The answer is not one fixed number because the volume is tied to the medication order, the device cup design, and the treatment goal, whether that goal is humidifying airways, thinning secretions, or delivering a prescribed medication.
A nebulizer for a baby should always be used under a clinician’s plan, especially for very young infants. In practice, teams choose a volume that allows the device to aerosolize steadily without drying out too early, while keeping treatment time reasonable for a baby who may not tolerate a long session. The safest approach is to follow the exact prescription on the medication label and confirm the device instructions for the minimum and recommended fill volume.
Why Saline Volume Matters for Infant Nebulizer Treatments
Saline volume matters because it affects how long aerosol output stays consistent during a session. Too little fluid can shorten run time and produce uneven delivery, which may leave the baby coughing or frustrated without completing the intended dose. Too much fluid can extend the session beyond what an infant can tolerate and may increase the chance of leakage or poor mask seal.
Clinicians also consider what is being delivered. If saline is being used as the carrier for a medication, the ordered dilution drives the volume. If saline is being used alone for airway moisture, the care team may choose a volume that supports a steady mist while keeping the baby calm. The goal is predictable output, not a long session that turns stressful.
Typical Fill Volumes and What Changes the Number
Most small-volume nebulizer cups have a practical working range, and many operate best once the cup is filled above the minimum level needed for stable aerosol generation. The exact number varies by brand and cup design, which is why clinicians check the device instructions rather than relying on a universal amount. When caregivers ask about “mL,” the most accurate answer is the prescribed volume on the medication order plus whatever the device requires to run consistently.
Several factors change the number in real use. Medication type, intended dose, and whether dilution is required all influence volume. The flow source matters too. A higher flow may aerosolize faster and shorten run time, while a lower flow may extend the session but reduce output strength. For a Nebulizer session to be predictable, the fill volume and the flow need to match the device’s expected operating range.
Practical Setup Checks for a Nebulizer for a Baby
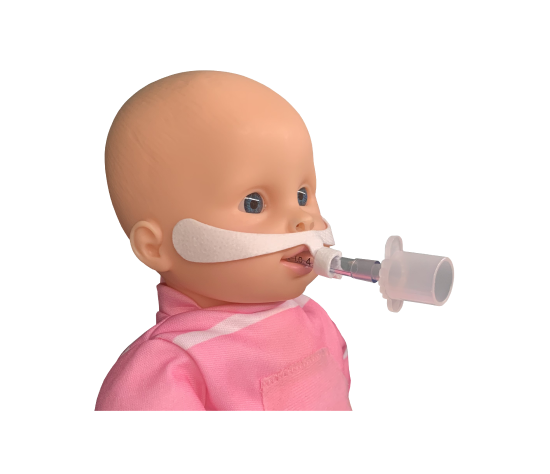
A safe setup starts with the basics that prevent common problems. Caregivers confirm the cup is seated correctly, tubing connections are snug, and the mask is the right size to avoid large leaks. Infants breathe mostly through the nose, so a poor seal can reduce delivery even when the machine is running. Positioning helps as well. A baby held upright or slightly elevated often tolerates the mist better and clears secretions more comfortably.
During the session, the best check is watching for steady mist and monitoring comfort. If output becomes weak early, it may be a low fill volume, a loose connection, or a flow issue. If the baby becomes more distressed, coughing increases, or breathing effort rises, the session should be paused and the care plan reviewed. For infant-specific safety questions, read Is Nebulizer Safe for 2 Month Old Baby to learn more.
When Nebulized Saline Is Used and When to Pause
Nebulized saline may be used to support airway moisture and secretion clearance in certain care plans, especially when congestion or thick secretions are part of the clinical picture. It is also used as a diluent when a medication order calls for a specific concentration or delivery time. In both cases, the plan should be guided by a clinician, because infants can worsen quickly if the underlying problem is not just congestion.
There are also clear moments to pause and ask for guidance. If a baby shows persistent increased work of breathing, poor feeding, color change, or worsening wheeze, the priority is assessment, not continuing aerosol at home. If the baby is a newborn or premature, the decision to use aerosol therapy should be even more structured. For age-related considerations, read Are Nebulizers Safe for Newborns? for more info.
B&B Medical Technologies Approach to Consistent Aerosol Therapy
B&B Medical Technologies supports respiratory care by focusing on reliable aerosol delivery in settings where patient tolerance and repeatable setup matter. In clinical workflows, teams rely on equipment that can provide steady output, predictable run time, and straightforward checks so therapy stays consistent from one session to the next. This emphasis on practical performance supports caregivers who need aerosol therapy to be manageable.
B&B Medical also works within a broader respiratory product landscape that includes devices used for different volumes and care environments. In facilities where higher volume delivery is part of a protocol, teams may compare approaches across equipment categories and monitoring habits. For context on how higher volume delivery fits into modern respiratory care, read Large Volume Nebulizer Revolutionizes Respiratory Care for a detailed understanding.
Frequently Asked Questions
The correct amount depends on the prescription and the nebulizer cup’s recommended fill range. Follow the ordered dose on the medication label and use the device instructions to confirm the minimum volume needed for steady mist.
Some care plans use saline to support airway moisture and secretion clearance, but infants should be assessed if breathing effort is increased. Follow pediatric guidance rather than trialing repeated treatments at home without a plan.
This can happen when the fill volume is too low, tubing is loose, or flow is not set correctly for the device. Recheck the cup, connections, and prescribed setup before restarting.
Treatment time depends on the device, flow source, and how much fluid is placed in the cup. Many plans aim for a session length that the baby can tolerate while still delivering the ordered dose.
Stop if the baby becomes more distressed, breathing effort increases, feeding worsens, or symptoms escalate instead of improving. Infants can change quickly, so worsening signs should be reviewed by a clinician.